

The perfect examples of progress notes are SOAP. Summary of the diagnosis, functional status, symptoms and the progress to the current.The results obtained from the clinical tests.The frequency at which the treatment has been furnished to the patient.The required medication that has been prescribed and the results that have been derived from such prescription.Besides this, progress notes also keep a record of the methodologies that have been implemented by the practitioner to take care of any undue crisis that might have arisen in the midst of the procedure.ĭeveloping a progress note requires numerous forms of data. There are various components which go ahead in creating a progress note including the assessment, diagnosis and the treatment protocols involved in the procedure. In counselling, progress notes are used to measure the progress of a particular treatment being administered. No rubs.ĭiagnosis: Usage of antacids and H2 blockers.ĭiagnostic – Avoid food that makes symptoms worse.Ĭonsultation – Seek medical advice if symptoms seem to worsen.įollow-up – Return again if treatment needs to be further assessed by the doctor.ĭate – _ Progress Notes in Counseling Physical Examinations: Abdomen is soft and protuberant. Social History/Habits: Denies smoking, drinking or drug use. History of Present Illness (HPI): “Burning feeling started two months ago. Generally healthy.Ĭhief Complaint (CC): “Burning feeling in the stomach.” Self-Care Plan: _ĭoctor’s Signature: _ĭate: _ Example for SOAP Notes for Counseling Modalities Applied: _Ĭhanges Achieved: _ĭiagostics: _ Patient’s Name: _ Date: _Ĭlient Compliants : _ Physical Examinations: (Include only those examinations which are relating to the chief complaint)ĭiagnostic: (List of results that you already have)ĭiagnosis: (The Diagnosis should be written according to the level of your understanding of the problem and the subjective and objective data)ĭiagnostic – (In this part, you have to write about the X-rays, lab and other tests that you plan for the patient)ĭoctor’s Signature – _ General Observations: (Does the patient appear to be in anxiety, pain or any other observation can be noted down here) Vital Signs: (Vital Signs that haven’t been listed elsewhere) Social History/Habits: (Social habits such as smoking, consumption of tobacco, drugs, alcohol etc. of any past occurrences of the present illness)Ĭurrent Medications: (Include all the medications that the patient is taking) History of Present Illness (HPI): (Include details such as onset, duration, progression, timing etc.
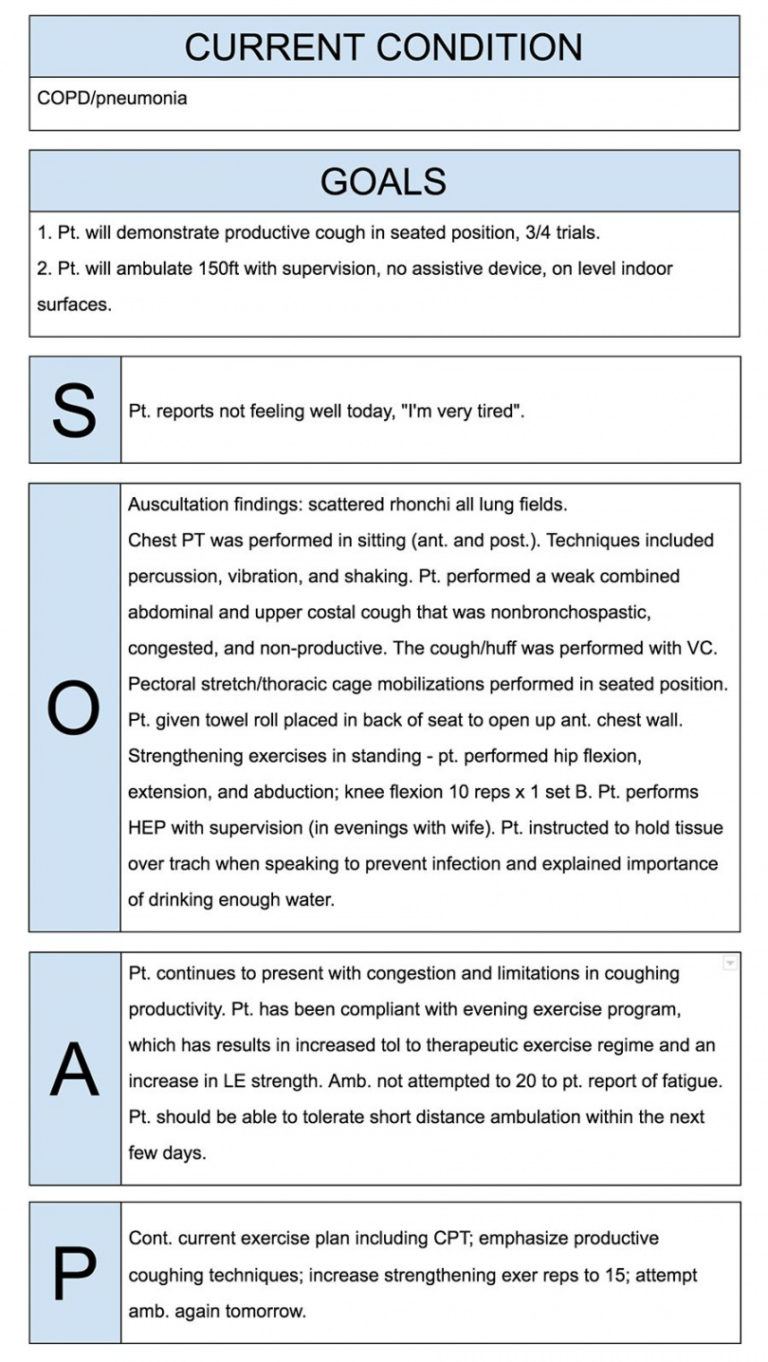

ID: (Brief details regarding the patient)Ĭhief Complaint (CC): (Use patient’s primary report in the form of direct quotes in quotation marks) Given below, are few SOAP note templates which can be used in counselling. Needs support for dealing with (the situation)– Needs to take responsibility for being on time to the group meetings.ĥb21e1456b55a.php SOAP Samples SOAP Note Template for Counseling.A few samples for which could be included in this section are: Even the most obvious of the assessments are not excluded. Various other factors could also be included in this section such as details about the session, situation etc. Assessment – The Assessment section contains a judgment of the situation that the patient is going through.Intraoral – Eruption of the supra, occlusion on the pericoronal tissues, fetid odour, pain to palpation etc. Clinical Exam Results: Extraoral – No symmetry or swelling.Most commonly, this section houses the various changes or problems which the client has been going through. Objective – The Objective sections contains data which matches with the statement, previously made by the client.But it has been difficult as I just quit smoking.” “I start to break down when he yells at me.“My lower jaw has been hurting for a couple of days.”.Traditionally, this statement is preferred to be recorded in the form of a direct quote. Subjective – The Subjective section contains a summary statement that is given by the client.Given below are a few sample statements which can be used while developing a SOAP note.
Soap notes how to#


 0 kommentar(er)
0 kommentar(er)
